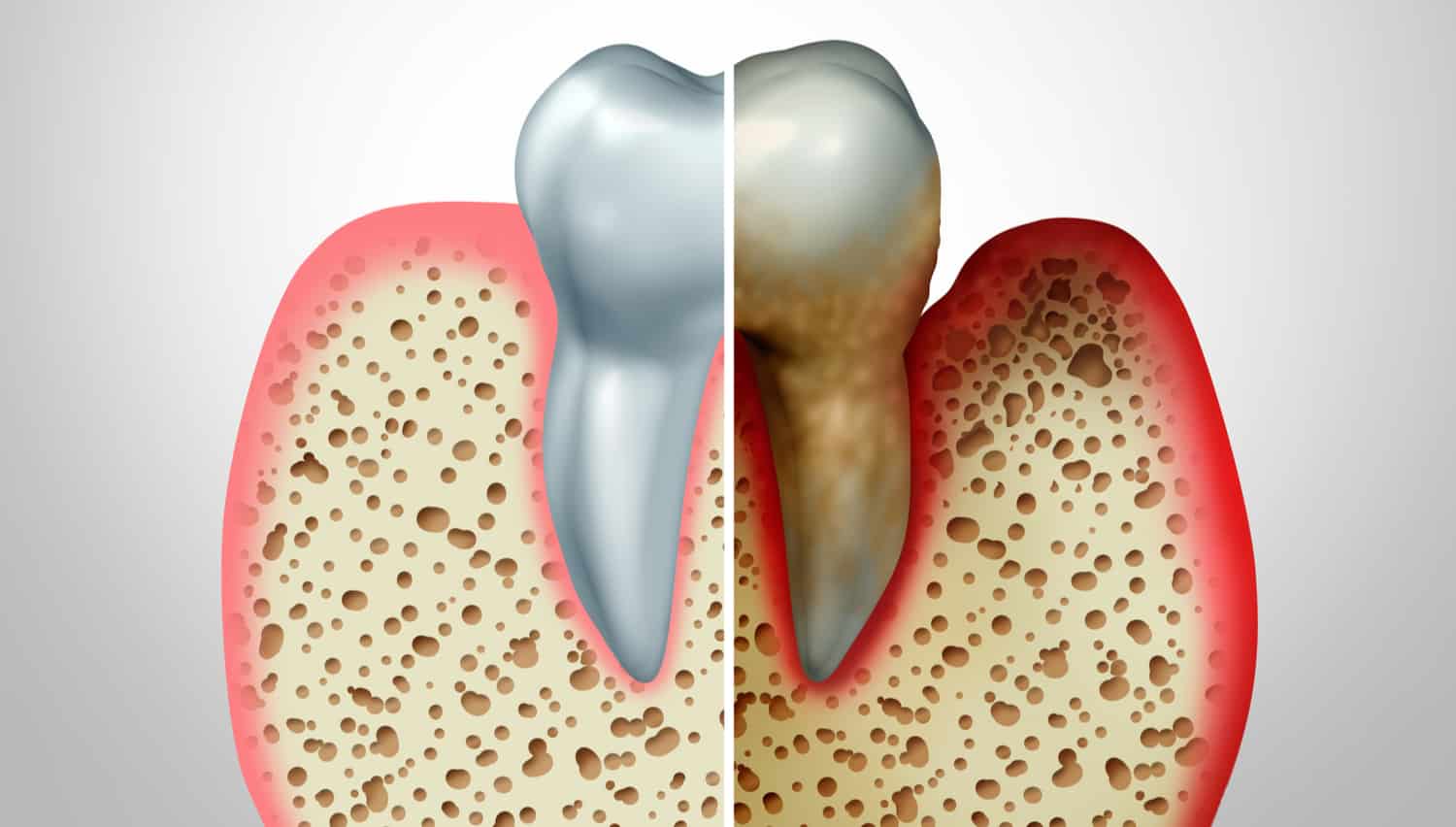
Initial signs rarely involve bone. Gum tissue may recede as inflammation continues around the teeth. This recession often exposes tooth roots. The exposed surface becomes more sensitive to temperature. Food may collect in pockets that deepen gradually. These pockets trap bacteria under the gum line. Bleeding during brushing may follow. As inflammation spreads deeper, bone structure begins to react.
Chronic periodontitis triggers an immune response that damages supporting bone
The immune system turns defensive. Chronic periodontitis triggers an immune response that damages supporting bone. Bacteria release toxins below the gum surface. These toxins provoke cytokines and enzymes from immune cells. These chemical responses degrade connective tissue attachments. The jawbone responds by resorbing the weakened area. Over time, structural support for teeth diminishes. Bone loss begins silently and continues without pain.
Loss of attachment causes teeth to shift, loosen, or fall out
Tooth stability becomes compromised. Loss of attachment causes teeth to shift, loosen, or fall out. Chewing becomes uneven and difficult. Gaps may appear where teeth once aligned tightly. Bone no longer anchors roots securely. Implants may not succeed if bone loss continues. Bridges and dentures become harder to fit. Aesthetics and function are both altered significantly.
X-rays often reveal bone loss before symptoms are physically noticeable
Imaging provides early insight. X-rays often reveal bone loss before symptoms are physically noticeable. Vertical defects or horizontal reduction become visible on radiographs. Dentists compare current films to previous ones. Subtle changes may be missed without consistent monitoring. Deep pockets without visible recession should raise concern. Imaging is vital during periodontal evaluations. Early detection leads to more effective treatment options.
Advanced stages may require surgical intervention to remove infected tissue
Cleaning alone may not be enough. Advanced stages may require surgical intervention to remove infected tissue. Flap surgery exposes the roots and bone. This allows deeper cleaning and debridement. Some procedures include reshaping the bone. In severe cases, bone grafting is considered. Surgical regeneration aims to restore lost structure. Healing depends on infection control and oral hygiene.
Bone grafts use synthetic or biological materials to rebuild lost jaw structure
Regeneration requires a scaffold. Bone grafts use synthetic or biological materials to rebuild lost jaw structure. Some grafts come from the patient’s own body. Others use donated or lab-made material. The graft provides a framework for new growth. Over time, natural bone replaces the grafted area. This process restores height and density. It prepares the jaw for future restorative work.
Tissue loss around implants may also indicate underlying bone resorption
Implants face similar risks. Tissue loss around implants may also indicate underlying bone resorption. Peri-implantitis mirrors periodontal disease. Bacterial biofilms accumulate around the implant neck. Inflammation begins in the soft tissue and progresses deeper. Once the implant loses bone support, mobility increases. Immediate care prevents full implant failure. Regular maintenance visits reduce this risk.
Smoking significantly increases the speed and severity of periodontal bone damage
Lifestyle choices accelerate destruction. Smoking significantly increases the speed and severity of periodontal bone damage. Nicotine restricts blood flow to the gums. Healing slows after every insult or infection. Bacterial environments flourish under smoke exposure. Smokers often show fewer symptoms until late stages. Bone loss progresses silently behind healthier-looking tissue. Quitting improves blood supply and immune response quickly.
Diabetes may impair the body’s ability to respond to oral infections
Systemic conditions contribute silently. Diabetes may impair the body’s ability to respond to oral infections. High blood sugar encourages bacterial growth. It also impairs neutrophil activity and collagen repair. Wound healing becomes delayed or incomplete. Diabetics are prone to deeper pockets and faster bone loss. Glycemic control improves periodontal stability. Dental teams often coordinate with physicians during care.
Long-term maintenance requires routine cleaning, monitoring, and home care adjustment
Management is lifelong. Long-term maintenance requires routine cleaning, monitoring, and home care adjustment. Patients must adhere to strict oral hygiene. Antibacterial rinses may be prescribed after treatment. Scaling and root planing may recur periodically. Follow-ups track pocket depth and attachment levels. Small lapses allow pathogens to recolonize quickly. Consistency slows or halts bone resorption.
