Peri-0implantitis develops when bacteria damage the tissues around a dental implant, and treating it effectively requires understanding how inflammation begins, how bone reacts to infection, and how timely intervention protects both oral health and long-term implant success in a predictable and patient-friendly way.
Why does peri-implantitis develop around dental implants?
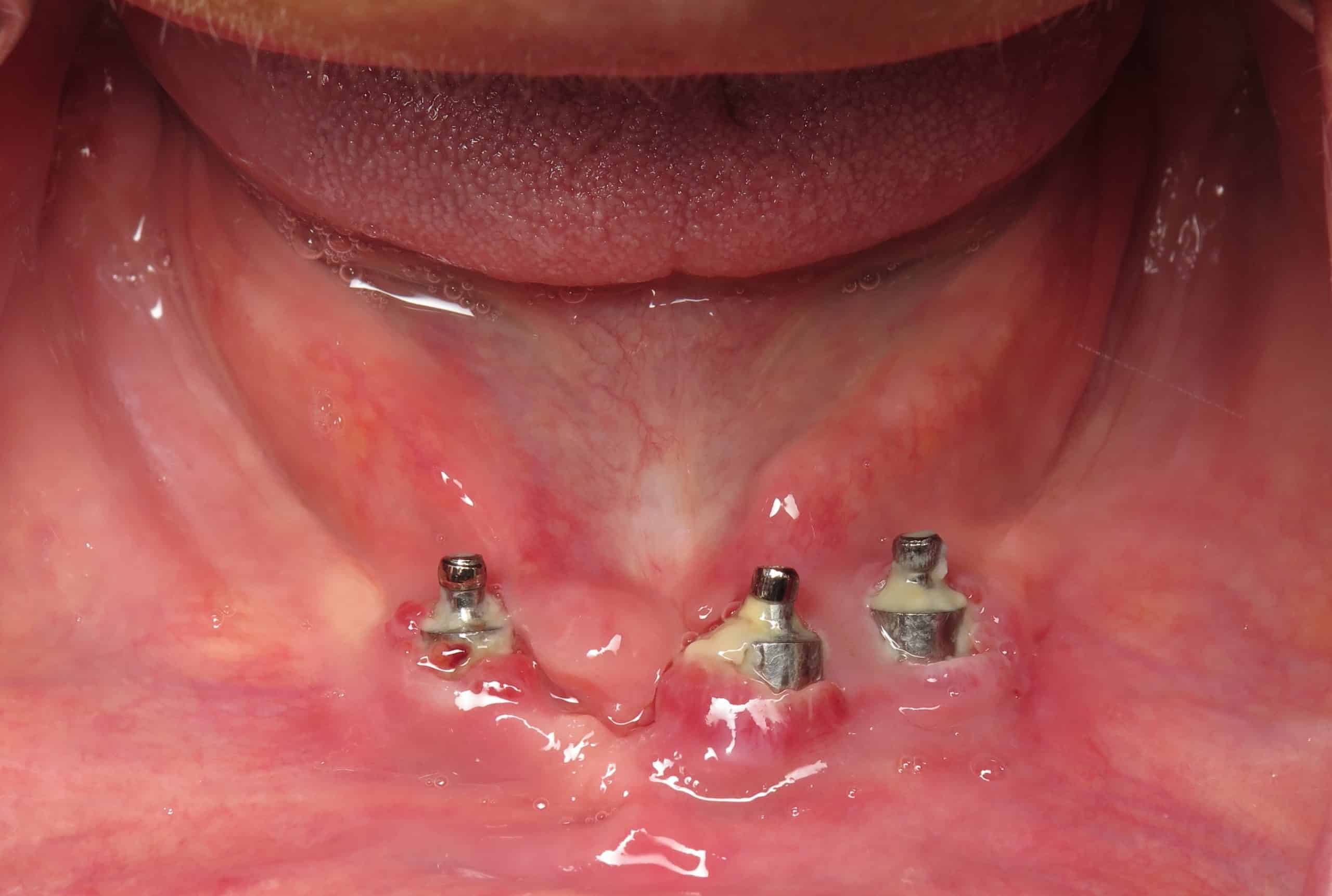
Peri-implantitis develops when plaque builds up around the implant surface. This buildup triggers inflammation in nearby tissues. According to our editor’s research, early signs often include bleeding, swelling, and tenderness. Many patients overlook these symptoms because they mimic mild gum irritation. The condition progresses when bacteria reach deeper layers. These bacteria disrupt the connection between the implant and surrounding bone. As a result, the tissues weaken steadily. Understanding this process guides treatment decisions. Early diagnosis improves outcomes significantly.
How does inflammation damage bone surrounding the implant?
Inflammation alters the body’s normal healing response. Instead of repairing tissue, inflammation breaks down bone. As a result of our editor’s reviews, bone cells become less active during infection. The immune system releases chemicals that weaken bone structure. These changes occur quietly over time. Patients often notice looseness or discomfort later. Once bone loss begins, the implant loses support. Treating inflammation quickly prevents long-term damage. Healthy bone remains essential for implant stability. Monitoring bone levels becomes a key part of care.
What early symptoms suggest urgent treatment?
Early symptoms help identify peri-implantitis before it progresses. Bleeding during brushing offers an early warning. According to our editor’s research, consistent swelling around the implant also signals trouble. Some patients notice a bad taste or persistent odor. These symptoms reflect bacterial activity. Increased sensitivity while chewing may follow. Color changes in the gums appear in advanced stages. Recognizing these early signs encourages timely treatment. Regular checkups help catch peri-implantitis early. Quick action limits tissue damage.
How does professional cleaning remove harmful bacteria?
Professional cleaning targets bacteria hidden around the implant. Special tools reach deep pockets that brushing misses. As a result of our editor’s reviews, ultrasonic devices break down stubborn plaque. These tools vibrate carefully to avoid damaging the implant. Antibacterial rinses support cleaning by reducing surface bacteria. Deep cleaning reduces inflammation significantly. Removing plaque also lowers future risk. This step becomes the foundation of treatment. Follow-up visits ensure the area stays stable.
Why do some cases require surgical intervention?
Surgery becomes necessary when cleaning alone cannot control infection. Severe bone loss often requires reshaping damaged areas. According to our editor’s research, surgeons remove inflamed tissue to allow healthy healing. Some procedures include adding bone grafts. These grafts support the implant and encourage new bone growth. Other techniques involve adjusting the implant surface. Surgery helps restore stability in advanced cases. Early planning ensures predictable results. Surgery offers lasting improvement when conservative care fails.
How do regenerative techniques support healing?
Regenerative techniques help rebuild lost tissue around the implant. These techniques encourage new bone to grow. As a result of our editor’s reviews, membranes protect graft materials during healing. These membranes separate healthy and unhealthy tissues. Growth factors stimulate natural repair. Regeneration strengthens the implant’s foundation. Healing continues over several months. Patients notice gradual improvement. Regenerative therapy works best when inflammation is controlled early. This approach protects long-term function.
Why does implant surface design affect treatment success?
Implant surfaces vary in texture and coating. These differences influence how bacteria attach. According to our editor’s research, rough surfaces attract more plaque. Smooth surfaces resist buildup better. Surface design also affects how bone integrates. Some designs encourage quicker healing. These differences shape treatment choices. Surgeons consider surface type before planning care. Matching treatment to implant design improves outcomes. Understanding these details strengthens long-term success.
How important is patient hygiene in controlling peri-implantitis?
Patient hygiene remains central to preventing peri-implantitis. Daily brushing removes surface bacteria. As a result of our editor’s reviews, interdental cleaning helps reach tight spaces. Gentle brushing around implants protects surrounding tissue. Consistent routines reduce inflammation risk. Patients play a major role in maintenance. Dental professionals offer guidance for problem areas. Good hygiene supports all treatment methods. It remains one of the most effective prevention tools.
Why do lifestyle factors influence implant health?
Lifestyle habits affect how tissues heal and respond to infection. Smoking reduces blood flow to the gums. According to our editor’s research, this slows healing and weakens bone. Uncontrolled diabetes also increases infection risk. Poor diet contributes to plaque buildup. Managing these factors strengthens treatment results. Healthy habits support stable implants. Patients benefit from discussing lifestyle concerns with their provider. Small adjustments improve long-term oral health.
How do follow-up visits ensure stable progress?
Follow-up visits track healing after treatment. Dentists measure pocket depth and assess soft tissue health. As a result of our editor’s reviews, imaging helps monitor bone levels. Early signs of relapse become easier to manage. These visits also adjust home-care recommendations. Regular monitoring supports lasting stability. Many patients benefit from visits every three to six months. Consistent evaluation protects implant health. Follow-up care offers reassurance during recovery.
